As an Amazon Associate I earn from qualifying purchases.
The 2024 ASCRS Guidelines emphasize a stepwise approach to hemorrhoid management. You'll start with conservative treatments like increasing fiber intake and fluid consumption. If these don't work, office-based procedures like banding are recommended for grade I-II internal hemorrhoids. For more advanced cases, surgical options like excisional hemorrhoidectomy may be necessary. Pain management focuses on multimodal regimens to minimize opioid use. The guidelines also address special populations, including pregnant women and patients with IBD or cirrhosis. By following these evidence-based recommendations, you'll be on the right track to effectively manage hemorrhoids and prevent recurrence. There's much more to explore in these exhaustive guidelines.
Diagnosis and Evaluation

The diagnosis and evaluation of hemorrhoids are essential steps in effective management. You'll need to undergo a disease-specific history and physical examination, focusing on the degree and duration of your symptoms and any risk factors. Your doctor will assess the severity of your hemorrhoids, which can be internal or external.
Rectal bleeding is a key symptom to evaluate, as painless bleeding during bowel movements often indicates internal hemorrhoids. Your medical history is pivotal in determining the best treatment plan, so be prepared to discuss factors like constipation, straining, prolonged sitting, and frequent bowel movements.
A thorough physical examination helps identify the severity of your hemorrhoids and guides treatment decisions. In some cases, your doctor may recommend an exhaustive endoscopic evaluation of your colon, especially if you're experiencing symptomatic hemorrhoids with rectal bleeding.
Accurate diagnosis is essential for developing an effective treatment plan. By providing detailed information about your symptoms and undergoing an in-depth evaluation, you'll help your healthcare provider make the best decisions for managing your hemorrhoids.
Conservative Management Approaches
How can you manage hemorrhoids without resorting to surgery? The latest ASCRS guidelines emphasize conservative management approaches as the first line of defense for patients with symptomatic hemorrhoidal disease. Dietary and behavioral modifications are strongly recommended, backed by moderate-quality evidence. You should increase your fiber intake, as studies show it can reduce the risk of persistent symptoms by 53%. Additionally, boost your fluid consumption to manage hemorrhoid symptoms effectively.
These changes can help prevent constipation, straining, and frequent bowel movements, which often exacerbate the condition. For further relief, medical therapy is conditionally recommended. While based on low-quality evidence, it offers minimal harm and may provide symptomatic relief.
If conservative treatment doesn't yield results, especially for grade 1 or 2 symptomatic hemorrhoids, office-based procedures like rubber band ligation (RBL) are recommended. This technique, also known as hemorrhoid banding, can also benefit select patients with grade 3 hemorrhoids who haven't responded to other approaches. By following these guidelines, you can effectively manage your hemorrhoids and potentially avoid more invasive interventions.
Office-Based Procedures

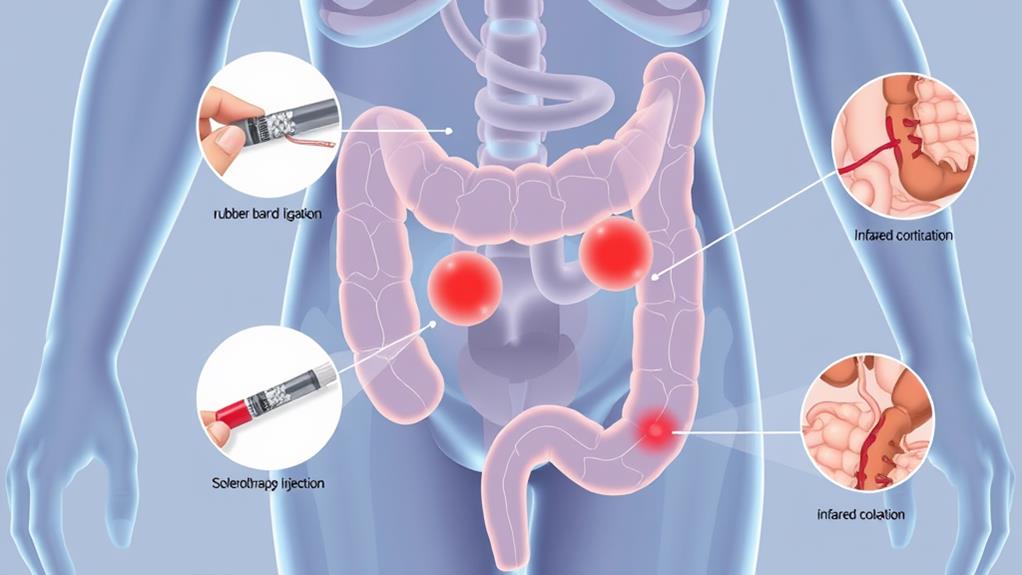
Office-based procedures offer effective, less invasive alternatives for treating internal hemorrhoids when conservative measures fail. You'll find that hemorrhoid banding is often the most successful option, with success rates up to 80%. Other treatments like sclerotherapy and infrared coagulation can also be effective for grade I-III internal hemorrhoids, providing you with multiple choices based on your specific condition.
Banding for Internal Hemorrhoids
Among office-based procedures for internal hemorrhoids, banding stands out as the most effective option for symptomatic grade I-II cases. The American Society of Colon and Rectal Surgeons (ASCRS) guidelines strongly recommend this technique for patients with grade I-II internal hemorrhoids who haven't responded to conservative treatment. You'll find that hemorrhoid banding offers significant symptomatic relief with minimal risk, making it an attractive choice over more invasive surgical options.
If you're dealing with symptomatic hemorrhoids and medical treatments haven't worked, your doctor might suggest office-based procedures like banding, sclerotherapy, or infrared coagulation (IRC). Banding, however, is often the go-to choice due to its effectiveness. It's typically performed in a doctor's office or clinic, making it convenient and less intimidating than surgery.
The ASCRS guidelines also indicate that banding can be suitable for select patients with grade III hemorrhoids who haven't responded to conservative measures. While the evidence quality is considered low, the guidelines conditionally recommend banding based on its proven ability to provide symptomatic relief. As you explore treatment options, consider discussing hemorrhoid banding with your healthcare provider to determine if it's right for you.
Sclerotherapy Treatment Options
Sclerotherapy offers another effective office-based treatment for internal hemorrhoids, particularly for those that haven't responded to conservative measures. This minimally invasive procedure involves injecting a solution directly into the hemorrhoid tissue, causing it to shrink and eventually fall off. You'll typically undergo sclerotherapy in your doctor's office, with sessions lasting 30 minutes to an hour.
The American Society of Colon and Rectal Surgeons recognizes sclerotherapy as a viable option for hemorrhoid management, especially for small to medium-sized internal hemorrhoids. Success rates range from 70% to 90%, making it a compelling alternative to other treatments like hemorrhoid banding or hemorrhoid artery ligation. While you may experience some discomfort, bleeding, or infection, it's generally considered safe.
If you're dealing with symptomatic hemorrhoids or rectal bleeding, sclerotherapy could be an appropriate treatment option. However, it's worth mentioning that multiple sessions may be required for ideal results. Your doctor will assess the size and location of your hemorrhoids to determine if sclerotherapy is the best course of action for your specific case.
Infrared Coagulation Effectiveness
Infrared coagulation (IRC) stands out as another effective office-based procedure for treating internal hemorrhoids. You'll find that IRC is particularly useful for grade I and II internal hemorrhoids, with a reported success rate of 70-90% in reducing symptoms and preventing recurrence. The American Society of Colon and Rectal Surgeons (ASCRS) recommends IRC as a viable treatment option, citing its effectiveness and low risk of complications.
A study in Diseases of the Colon and Rectum revealed that IRC effectively reduced bleeding and symptoms in 85% of patients, with a low 5% complication rate. You might appreciate that IRC is often preferred over other office-based procedures due to its minimal discomfort and rapid recovery time. It's an attractive option if you're looking to avoid surgery or more invasive treatments.
For ideal hemorrhoid management, IRC can be combined with other office-based procedures like rubber band ligation. This versatility makes it a valuable tool in your treatment arsenal. With its ease of use and high success rate, IRC continues to be a cornerstone in the ASCRS guidelines for managing internal hemorrhoids effectively and safely.
Surgical Treatment Options
For patients with advanced or complex hemorrhoids, surgical interventions offer effective treatment options. Excisional hemorrhoidectomy is recommended for select patients with external hemorrhoids or those with symptomatic grade 3-4 internal and external hemorrhoids. This procedure is particularly useful if you've failed or can't tolerate office-based treatments.
Doppler-guided hemorrhoidal artery ligation (HAL) is an alternative for internal hemorrhoids. It results in less pain but has higher recurrence rates compared to excisional hemorrhoidectomy. However, stapled hemorrhoidopexy (SH) isn't recommended as a first-line surgical treatment due to its marginal efficacy and significant risks.
If you're dealing with thrombosed external hemorrhoids, early surgical excision may be beneficial in select cases. One key consideration is that surgical excision is effective for patients who aren't candidates for office-based procedures or have concomitant external hemorrhoidal disease.
When considering surgical options, discuss the benefits and risks with your healthcare provider. They'll help determine the most appropriate treatment based on your specific condition, symptoms, and overall health status. Remember, the goal is to provide long-lasting relief while minimizing complications and recurrence.
Pain Management Strategies

You'll want to employ a multimodality pain regimen to reduce narcotic usage and promote faster recovery after surgical hemorrhoidectomy. Consider incorporating fiber supplements, as they've been shown to substantially reduce the risk of persistent symptoms. You can also opt for advanced surgical techniques like bipolar energy devices or ultrasonic shears, which are associated with less postoperative pain and faster recovery compared to traditional methods.
Multimodal Pain Relief Approaches
Managing pain effectively after hemorrhoid surgery is essential for patient comfort and recovery. The ASCRS guidelines recommend a multimodal pain regimen for patients undergoing surgical hemorrhoidectomy. This approach combines different types of medications to reduce opioid use and promote faster recovery.
You'll likely be prescribed a combination of acetaminophen, NSAIDs, and muscle relaxants to manage your postoperative pain. This multimodal approach minimizes the need for narcotic pain relievers, reducing the risk of respiratory depression and other opioid-related side effects. Research has shown that this combination can substantially decrease opioid use while improving patient satisfaction.
Your doctor may also consider using liposomal bupivacaine, a long-acting local anesthetic that can provide pain relief for up to 72 hours after surgery. This can further enhance your comfort during the initial recovery period.
When you're discharged, you'll receive instructions for continuing your multimodal pain management at home. It's imperative to follow these guidelines carefully to guarantee effective pain control and a smoother recovery process. By adhering to this thorough approach, you'll be better equipped to manage your pain effectively while minimizing potential complications.
Minimizing Opioid Usage
While opioids have traditionally been used for post-surgical pain management, the ASCRS guidelines now emphasize minimizing their usage following hemorrhoidectomy. Instead, they recommend a multimodal pain management approach to reduce narcotic usage and promote faster recovery. You'll benefit from a combination of medications, including nonsteroidal anti-inflammatory drugs, acetaminophen, and muscle relaxants. The ASCRS suggests using ketorolac, acetaminophen, and ibuprofen to manage postoperative pain effectively.
Regional anesthesia, such as local anesthetic injections or nerve blocks, can also play a vital role in your pain regimen. By implementing these strategies, you can greatly reduce your opioid usage – studies have shown up to a 50% reduction in opioid prescriptions with a multimodal approach.
Here's why minimizing opioid usage is vital:
- You'll experience fewer side effects and risks associated with opioids
- You'll recover faster and return to normal activities sooner
- You'll reduce the risk of developing opioid dependence
- You'll contribute to combating the opioid epidemic
- You'll experience more effective pain relief through targeted treatments
Recurrence Prevention
Preventing recurrence of hemorrhoids is a crucial aspect of long-term management. The American Society of Colon and Rectal Surgeons (ASCRS) recommends adopting lifestyle changes to reduce the risk of recurrence. Increasing your fiber intake is a key strategy, with studies showing it can lower the risk of persistent symptoms by 53%. You should also boost your fluid consumption to complement the increased fiber intake.
For symptomatic grade 1 or 2 hemorrhoids, office-based procedures like rubber band ligation can be effective in preventing recurrence. If you're dealing with more advanced cases, surgical interventions may be necessary. Excisional hemorrhoidectomy has shown promising results, with a low recurrence rate of 5.4% after one year. However, newer techniques like Doppler-guided hemorrhoid artery ligation (HAL) may have higher recurrence rates, with one study reporting 23.1% at one-year follow-up.
To minimize your risk of recurrence, follow your doctor's recommendations for lifestyle modifications and consider the appropriate treatment options based on the severity of your condition. By combining these strategies, you can substantially reduce the likelihood of hemorrhoid recurrence and improve your long-term quality of life.
Special Patient Populations

Three special patient populations require unique considerations in hemorrhoid management: pregnant women, patients with inflammatory bowel disease (IBD), and those with cirrhosis. For pregnant women, conservative treatment is preferred, focusing on dietary changes and topical treatments. Surgical interventions are generally avoided unless absolutely necessary. IBD patients often experience symptomatic hemorrhoids due to chronic inflammation, and treatment should be coordinated with their gastroenterologist. Cirrhotic patients may have an increased risk of bleeding, so careful evaluation is vital before any invasive procedures.
Health care workers should be aware of these special considerations:
- Pregnant women may develop thrombosed external hemorrhoids due to increased pelvic pressure
- IBD patients might require more frequent follow-ups to monitor for complications
- Cirrhotic patients may need additional precautions during surgical treatment
- Grade III hemorrhoids in these populations might benefit from infrared coagulation (IRC) as a less invasive option
- Risk factors unique to each group must be carefully evaluated before treatment selection
For all special populations, a tailored approach is essential. You'll need to weigh the benefits and risks of each treatment option carefully. Conservative treatments should be exhausted before considering surgical interventions. Always consult with specialists familiar with these conditions to guarantee the best possible outcomes for your patients.
Future Research Directions
As the field of hemorrhoid management continues to evolve, researchers and clinicians must focus on several key areas to improve patient care. The American Society of Colon and Rectal Surgeons (ASCRS) emphasizes the need for comparative effectiveness studies of different treatment modalities, including both surgical and nonsurgical options. You'll find that future research directions should aim to determine the ideal treatment approach for patients, exploring the potential of combined therapies and their impact on patient-centered outcomes.
Cost-effectiveness studies are vital to inform healthcare policy and resource allocation decisions. You should also expect ongoing investigation into new technologies and minimally invasive procedures to establish their safety and efficacy. Research on preventing and managing hemorrhoid recurrence is another critical area that requires further exploration. Additionally, the development of biomarkers for predicting hemorrhoid risk and severity could revolutionize patient care.
Frequently Asked Questions
What Is the New Treatment for Hemorrhoids?
Like a beam of hope, laser therapy shines as a cutting-edge, non-surgical option for hemorrhoids. You'll find quick relief with this minimally invasive, office-based treatment. It's a same-day procedure offering rapid recovery and pain relief.
What Are the Management Guidelines for Haemorrhoids?
If you're dealing with hemorrhoid symptoms, start with dietary changes and lifestyle modifications. Improve your bowel habits and try conservative management. For persistent issues, consider early interventions like rubber banding or sclerotherapy. Patient education is vital throughout the process.
What Is the New Procedure for Hemorrhoidectomy?
You'll find new hemorrhoidectomy procedures are minimally invasive and laser-assisted. Stapled hemorrhoidectomy in the anal canal reduces painful recovery. These surgical techniques aim to minimize rectal bleeding, improve bowel habits, and lower complication rates. Postoperative care is vital for success.
What Are the Practice Guidelines for Hemorrhoids?
You'll start with a thorough exam to diagnose hemorrhoid symptoms and grade. Patient education focuses on prevention. Treatment options range from lifestyle changes to office procedures and surgery, depending on hemorrhoid classification and patient-specific factors.
Conclusion
You've now explored the latest ASCRS guidelines for hemorrhoid management. From diagnosis to surgical options, you're equipped with cutting-edge knowledge to tackle this common condition. Remember, prevention is key, and tailored approaches for special populations are vital. As you navigate these recommendations, keep in mind that the field is ever-evolving. Like a ship sailing through uncharted waters, stay vigilant for new research that may further refine these guidelines in the future.
Amazon and the Amazon logo are trademarks of Amazon.com, Inc, or its affiliates.