As an Amazon Associate I earn from qualifying purchases.
When deciding between hemorrhoid banding and surgery, consider your condition's severity and personal preferences. Banding is a minimally invasive option for internal hemorrhoids, offering quick recovery and high success rates. It's generally painless and cost-effective. Surgery, while more invasive, can be more effective for severe cases but requires longer recovery. Your doctor will evaluate your hemorrhoid grade and medical history to recommend the best option. Factors like pain tolerance, time off work, and insurance coverage also play a role. Understanding the pros and cons of each treatment will help you make an informed decision for lasting relief.
Understanding Hemorrhoids
Hemorrhoids, often referred to as "piles," are swollen blood vessels in the lower rectum and anus. These swollen veins can occur inside the anal canal (internal hemorrhoids) or around the anus (external hemorrhoids). You may experience discomfort, itching, or bleeding during bowel movements if you have hemorrhoids.
Several factors can contribute to the development of hemorrhoids, including chronic constipation, straining during bowel movements, pregnancy, and prolonged sitting. As you age, your risk of developing hemorrhoids increases due to weakening tissues supporting the veins in your rectum and anus.
Internal hemorrhoids are classified into four grades based on their severity. Grade I hemorrhoids bulge into the anal canal but don't prolapse. Grade II protrude during bowel movements but retract on their own. Grade III require manual repositioning, while Grade IV remain permanently prolapsed.
It's important to understand that hemorrhoids are a common condition affecting millions of people worldwide. While they can be uncomfortable and sometimes painful, most cases can be managed with conservative treatments. However, if your symptoms persist or worsen, you may need to weigh the pros and cons of more advanced treatment options like banding or surgery.
Hemorrhoid Banding Explained
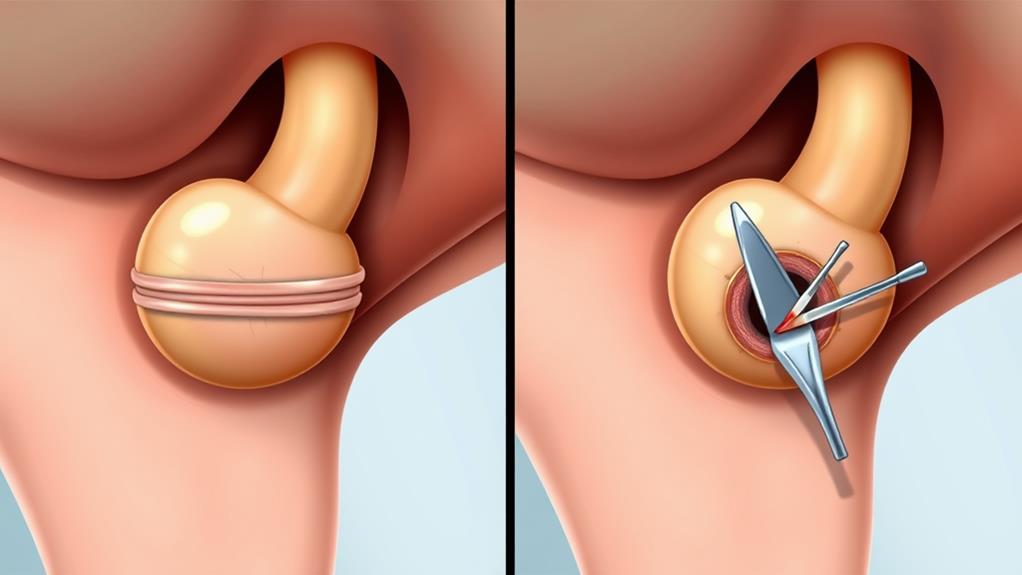
For many individuals suffering from hemorrhoids, banding offers a minimally invasive solution that can provide long-lasting relief. This hemorrhoid treatment, also known as rubber band ligation, is a quick and effective procedure your doctor may recommend for internal hemorrhoids.
During the procedure, a small rubber band is placed around the base of the hemorrhoid to cut off blood flow. This causes the hemorrhoid to shrink and eventually fall off within a week. The process typically takes just a few minutes and doesn't require anesthesia, making it one of the most convenient minimally invasive procedures available.
| Method | Success Rate | Effectiveness | Procedure Time |
|---|---|---|---|
| Traditional | 70-97% | Variable | Few minutes |
| CRH O'Regan | 99% | Proven | Few minutes |
Hemorrhoid banding is particularly effective for prolapsed or symptomatic hemorrhoids, offering relief from pain, bleeding, itching, swelling, and soiling. It's a long-term solution that can notably improve your quality of life. With success rates ranging from 70% to 99%, depending on the technique used, it's no wonder that millions of patients have chosen this treatment option.
Surgical Options for Hemorrhoids

While banding offers a minimally invasive solution, some cases of hemorrhoids require more extensive treatment. Hemorrhoid surgery, specifically hemorrhoidectomy, is often recommended for severe cases that don't respond to non-surgical options. This surgical removal procedure can be performed under local or general anesthesia and typically takes 30-60 minutes to complete.
During a hemorrhoidectomy, your surgeon will remove the problematic hemorrhoids, either internally or externally. It's usually an outpatient procedure, but you may need to stay in the hospital for a few hours or overnight for observation. While highly effective in relieving symptoms, hemorrhoidectomy does come with a longer recovery time of 2-4 weeks. You'll likely experience pain, discomfort, and some bleeding during this period, but these can be managed with pain medication and stool softeners.
It's important to note that hemorrhoidectomy, like any surgery, carries some risks. Complications such as infection, bleeding, and anal stenosis can occur in up to 5% of cases. Another surgical option is stapled hemorrhoidectomy, which may offer a quicker recovery time. Discuss these options with your doctor to determine the best approach for your specific case.
Comparing Effectiveness and Recovery
When it comes to treating hemorrhoids, the choice between banding and surgery often hinges on effectiveness and recovery time. Hemorrhoid banding boasts an impressive success rate of 70% to 97%, depending on the technique and hemorrhoid grade. It's a painless procedure with a quick recovery time, allowing you to return to normal activities within days.
On the other hand, hemorrhoidectomy, while having a low complication rate, requires a longer recovery period of 2 to 6 weeks. It can be painful, often necessitating pain medication during recovery. However, it's typically reserved for more severe cases.
If you're unfit for surgery or have conditions that contraindicate anesthesia, hemorrhoid banding is recommended as the first-line treatment. It's generally more cost-effective due to its non-invasive nature and shorter recovery time.
Consider your specific circumstances when choosing between these options. While banding offers a quicker, painless solution with high success rates, surgery might be necessary for more severe cases. Discuss with your doctor to determine which treatment aligns best with your health needs and lifestyle, weighing factors like recovery time, pain tolerance, and the severity of your condition.
Risks and Complications
With respect to risks and complications, hemorrhoid banding generally offers a safer profile compared to surgery. You'll face fewer risks of bleeding, infection, and reactions to anesthesia when opting for banding. The most common side effect you might experience is pain, which can be managed with over-the-counter pain relievers and stool softeners.
While hemorrhoid banding isn't without risks, they're relatively rare. In contrast, hemorrhoidectomy carries a higher complication rate, with about 15% of patients experiencing issues. More severe complications can affect up to 5% of surgical patients.
| Aspect | Hemorrhoid Banding | Hemorrhoidectomy |
|---|---|---|
| Common complications | Pain | Pain, bleeding |
| Risk of infection | Lower | Higher |
| Anesthesia-related risks | Minimal | Higher |
It's important to note that while banding may cause rare complications like urinary retention or anal stenosis, hemorrhoidectomy can lead to more serious issues. For instance, fecal incontinence affects up to 28% of surgical patients. When considering your treatment options, discuss these risks with your doctor to make an informed decision based on your specific condition and health status.
Candidacy for Each Treatment
When considering hemorrhoid treatment options, you'll need to assess the severity of your condition and evaluate your medical history. Your doctor will examine the grade and location of your hemorrhoids, as well as any symptoms you're experiencing. They'll also review your overall health, including any existing medical conditions or risk factors that could impact your eligibility for certain treatments.
Assessing Hemorrhoid Severity
Determining the severity of hemorrhoids is essential in deciding between banding and surgery as treatment options. Your doctor will evaluate your condition using a grading system that ranges from Grade I to Grade IV, with each grade indicating a different level of severity.
Grade I hemorrhoids involve bleeding without prolapse, while Grade II hemorrhoids prolapse but reduce on their own. If you have Grade III hemorrhoids, you'll experience prolapse that requires manual reduction. The most severe, Grade IV hemorrhoids, are irreducible and incarcerated.
Your doctor will carefully examine your anal area to evaluate the extent of prolapse and bleeding. This examination is pivotal in recommending the most appropriate treatment. If you have second-degree hemorrhoids, you're likely a candidate for rubber band ligation. However, if you're diagnosed with third-degree hemorrhoids, your doctor may suggest hemorrhoidectomy.
The choice between banding and surgery isn't always straightforward. It depends on various factors, including the severity of your hemorrhoids and your overall health. By accurately evaluating the grade of your hemorrhoids, your doctor can help you make an informed decision about which treatment option is best suited for your specific case.
Medical History Evaluation
A thorough medical history evaluation plays a key role in deciding whether you're a suitable candidate for hemorrhoid banding or surgery. Your doctor will assess various factors to determine the most appropriate treatment for your condition.
During this evaluation, you'll be asked about any existing medical conditions, previous surgeries, or ongoing treatments. Certain conditions, such as anal fissures, inflammatory bowel disease, or unexplained rectal bleeding, may rule out these procedures. If you have a history of cardiovascular disease or bleeding disorders, or if you're taking blood thinners, surgery might pose increased risks.
Your doctor will also perform a physical examination, including a digital rectal exam and anoscopy, to assess the severity and location of your hemorrhoids. This helps determine whether banding or surgery is more suitable for your case.
It's vital to provide a complete list of medications you're taking, as some may need to be discontinued before treatment. If you've had prior anal surgery, radiation therapy, or have pelvic floor dysfunction, your doctor will carefully evaluate your candidacy and may recommend a more tailored approach to address your specific needs.
Cost Considerations

Cost plays a crucial role in choosing between hemorrhoid banding and surgery. When considering your options, you'll find that hemorrhoid banding is generally more cost-effective than surgery. Banding typically costs between $500 and $1,500 per session, while a hemorrhoidectomy can range from $3,000 to $10,000 or more. The exact cost of surgery depends on factors like location, surgeon, and procedure type.
Insurance coverage can greatly impact your out-of-pocket expenses for both treatments. Many insurance plans cover at least part of the cost for banding and surgical procedures, but you must verify with your provider for specific details. Don't forget to factor in additional costs, such as follow-up appointments, pain management, or wound care, which can add to the overall expense of your treatment.
While cost is an important consideration, it shouldn't be the only factor in your decision-making process. Weigh the financial aspects against the potential benefits and risks of each treatment option. Consider your medical history, the severity of your condition, and your long-term health goals to make an informed choice between hemorrhoid banding and surgery.
Long-Term Outcomes
When considering long-term outcomes, both hemorrhoid banding and surgery offer significant relief for patients. Hemorrhoid banding has an impressive success rate ranging from 70-97%, depending on the technique used and hemorrhoid grade. For second-degree hemorrhoids, 64% of patients experience excellent improvement, while 20% see moderate improvement.
The CRH O'Regan System boasts a remarkable 99% success rate, making it an excellent choice for patients unfit for surgery or with conditions that contraindicate anesthesia. Banding produces a mucosal ulcer that heals through cicatrisation, fixing the mucosa to underlying skin. This process prevents hemorrhoid descent during defecation, resulting in long-term relief from symptoms.
For third-degree hemorrhoids, hemorrhoidectomy achieves better results, with 92% of patients showing no prolapse post-procedure. However, one key consideration is that banding typically has fewer complications compared to surgery.
When deciding between these treatments, consider your specific hemorrhoid grade and overall health. Both options can provide lasting relief, but the best choice depends on your individual circumstances. Consult with your doctor to determine which approach is most suitable for your condition and to discuss potential recurrence within the years following treatment.
Making an Informed Decision

Making an informed decision about hemorrhoid treatment requires careful consideration of various factors. Your doctor will help you weigh the pros and cons of hemorrhoid banding and hemorrhoidectomy based on your specific condition and overall health.
Consider the following comparison:
| Factor | Hemorrhoid Banding | Hemorrhoidectomy |
|---|---|---|
| Procedure | Rubber band ligation | Surgical Ligation |
| Pain Level | Less pain | More pain |
| Recovery Time | Quicker | Longer |
| Effectiveness | Good for mild to moderate | Best for severe cases |
| Setting | Doctor's office | Hospital |
Hemorrhoid banding, also known as rubber band ligation, is a minimally invasive option that can be performed in your doctor's office. It's generally associated with less pain and fewer side effects compared to surgery. However, it may not be as effective for severe hemorrhoids.
Hemorrhoidectomy, on the other hand, is a surgical procedure that offers a more permanent solution for extensive hemorrhoids. While it has a longer recovery time and more potential side effects, it may be necessary for severe cases that don't respond to other treatments.
Ultimately, the best choice depends on your individual circumstances. Consult with your doctor to discuss your options and make an informed decision based on your specific needs and preferences.
Frequently Asked Questions
Is Banding or Surgery Better for Hemorrhoids?
When considering treatment options for hemorrhoids, you'll find that both banding and surgery offer symptom relief. Your choice depends on pain management needs, recovery time, and success rates. Consider alternative therapies before making a decision with your doctor.
What Is the Disadvantage of Hemorrhoid Banding?
Did you know 1 in 20 Americans suffer from hemorrhoids? Hemorrhoid banding has disadvantages: painful recovery, limited success, and it's often a temporary solution. You might face incomplete removal, high recurrence rates, and risk complications like bleeding or infection.
Is Rubber Band Ligation Better Than Hemorrhoidectomy?
You'll find rubber band ligation often better for mild hemorrhoids. It's a quick, non-invasive office procedure with low risk factors and faster recovery. However, for severe cases, hemorrhoidectomy might provide more effective long-term pain relief as an outpatient treatment.
What Is the Most Effective Procedure for Hemorrhoids?
The most effective procedure for hemorrhoids depends on their grading and symptom severity. For severe cases, hemorrhoidectomy offers the best treatment outcomes. However, medical advancements like the CRH O'Regan System provide high patient satisfaction with less pain and faster recovery.
Conclusion
You're at a crossroads in your journey to heal those pesky hemorrhoids. Like choosing between a scenic route and a highway, banding and surgery each have their merits. Weigh the pros and cons carefully, considering your unique situation. Remember, there's no one-size-fits-all solution. Armed with knowledge, you're now ready to make an informed decision. Consult your doctor, listen to your gut, and take the path that'll lead you to comfort and relief.
Amazon and the Amazon logo are trademarks of Amazon.com, Inc, or its affiliates.
